Vidalia Urologist Highlights Strides in Treating Prostate Cancer
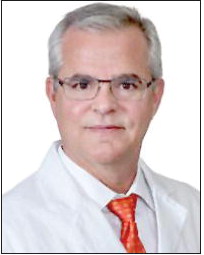
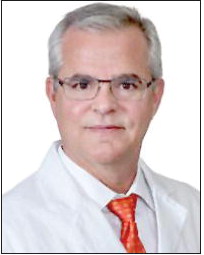
September Is National Prostate Cancer Awareness Month
On a global basis, prostate cancer is the second most commonly occurring cancer in men and the fourth most common cancer overall, according to the World Cancer Research Fund International (WCRF).
Based in London, the WCRF examines how diet, weight and physical activity affect the risk of developing and surviving cancer. As part of an international network of charities, WCRF has been funding life-saving research, influencing global public health policy, and educating the public since 1982.
In 2020, 1.4 million new cases of prostate cancer were reported worldwide. The good news is that in the United States, there is a 98% survival rate for men who are treated for localized prostate cancer. This fact is due to early detection and progressive treatment techniques.
Dr. Gilbert Gonzalez, a urologist practicing at Memorial Health Meadows Hospital in Vidalia, commented on changes in the way prostate cancer is now treated compared to the methods used when he began his practice 34 years ago.
Dr. Gonzalez earned his medical degree at the Medical College of Georgia in 1983 and completed his urology training in 1989. He first came to Vidalia in 2001, worked in Covington for a few years, and returned to Meadows in 2021.
During his years of practice, Dr. Gonzalez has witnessed many positive developments in the treatment of prostate cancer. “Treatments have vastly improved with radiation and the aiming capability of computers —specifically CT scans. Treatments are not as dangerous now and complications are lower.” Better efficacy and lower morbidity in treatment techniques might also be attributed in part to the use of robotically assisted targeted surgery.
The number of cases of prostate cancer has risen in step with the world’s population increase. In the U.S., about a quarter of a million cases are reported each year, and 35,000-40,000 prostate cancer deaths are recorded annually. “There is a high incidence of prostate cancer, and if a man lives to be 90, there will be a greater than 50% chance that prostate cancer will be found at his autopsy,” Dr. Gonzalez said.
But in actuality, the survival rate for localized prostate cancer is quite good, Dr. Gonzalez stressed. “Once it is diagnosed, if the cancer is localized to the gland and has not spread, the survival rate is high.”
Localized prostate cancer treatment is done with Brachytherapy, a radiation treatment that is given directly into the body and placed as close to the cancer as possible. The radiation is administered using tiny devices such as wires, seeds, or rods filled with radioactive materials. These devices are called implants.
Brachytherapy allows doctors to use a higher total dose of radiation over a shorter time than is possible with external beam therapy. The radiation dose is focused on the cancer cells and does less damage to the nearby normal cells. This treatment may be done along with external beam therapy to help destroy tumor cells for certain types of cancer.
Drugs may used when cancer becomes resistant to treatment or has spread into tissues, bones and organs. “The scene for prostate cancer drugs has changed because of anti-androgens,” Dr. Gonzalez said. These drugs block androgen hormones, such as testosterone, and can be used for many purposes, like slowing prostate cancer and minimizing the masculinizing effects of certain hormones. “We can now treat individuals with a drug called Lupron and anti-androgens. The combination of these drugs is very effective.”
Dr. Gonzalez said little is known as to the actual cause of prostate cancer. He said there are a handful of genetic markers or genes associated with prostate cancer such as BRCA1 (BReast CAncer gene 1) and BRCA2 (BReast CAncer gene 2. These are genes that produce proteins that help repair damaged DNA. Everyone has two copies of each of these genes — one copy inherited from each parent. BRCA1 and BRCA2 are sometimes called tumor suppressor genes because when they have certain changes, called harmful (or pathogenic) variants (or mutations), cancer can develop.
BRCA1 and BRCA2 are strongly associated with inherited prostate cancer. “It can run in families,” Gonzalez said of the genetic trait. People who are overweight and who have Type 2 Diabetes and hypertension run a slightly higher risk of developing prostate cancer. Studies show that individuals who eat lots of fruits and vegetables and engage in regular aerobic exercise appear to diminish their chances of getting prostate cancer.
Studies in the U.S. have shown that African American men are 1.6 times more likely to develop prostate cancer; not only that, but they are more likely to have the more aggressive forms of the cancer. “We are doing everything we can as a urological association to find these men with prostate cancer in the early stages, treat them, and lower this mortality rate,” Dr. Gonzalez noted.
Most family practitioners are tuned into providing periodic screenings for prostate cancer for their patients. This can be done in the form of PSA screenings and digital rectal exams (DRE). “The screening is there. Only people who refuse to get tested are at risk,” Dr. Gonzalez pointed out.
PSA — or prostatespecific antigen — is a protein produced by normal, as well as malignant, cells of the prostate gland. The PSA test measures the level of PSA in the blood. For this test, a blood sample is sent to a laboratory for analysis.
The blood level of PSA is often elevated in people with prostate cancer. The PSA test was originally approved by the Food and Drug Administration (FDA) in 1986 to monitor the progression of prostate cancer in men who had already been diagnosed with the disease. In 1994, the FDA approved the PSA test to be used in conjunction with a DRE to aid in the detection of prostate cancer in men 50 years and older.
There are no warning signs for prostate cancer in its early stages. “Once you start having symptoms, you are almost in a losing position,” Dr. Gonzalez emphasized. At this stage, the cancer has probably spread. “If man is between 50 and 75, and has a strong family history of prostate cancer, or has females in his family with breast cancer, I strongly encourage him to get tested.”
The urologist emphasized, “Early screening is an excellent way to prevent bad outcomes. Once diagnosed, patients should begin appropriate treatments, and if the cancer has spread, a combined, team approach to treatment with a urologist, oncologist and radiation therapist, has been proven to be the best approach for long-term survival.”
A nd with the Low Country Cancer Treatment Center on Meadows’ Vidalia campus, all of this can be accomplished close to home.